You wake up one morning, reach to pick up your phone, and suddenly your lower back screams. A jolt of pain runs down your leg. You think: “Is this just a slipped disc? Do I need surgery?” These questions terrify many—but the answer lies somewhere between fear and hope.
Today, we’ll walk through what “herniated disc” and “slipped disc” really mean, how to tell when surgery becomes necessary, and how to choose the right path with confidence.
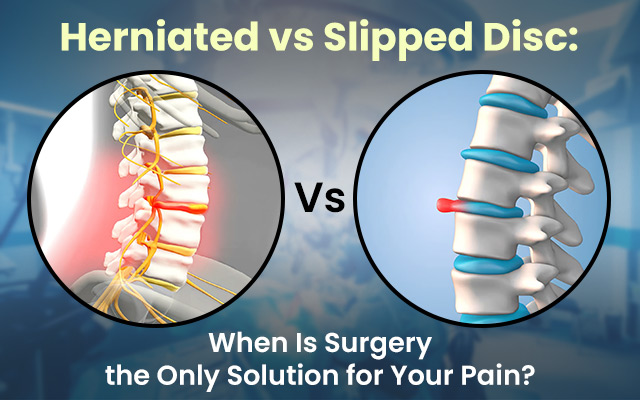
Understanding Disc Herniation and Slippage
What Is a Herniated Disc?
A herniated disc (also called a disc herniation) happens when the soft inner part of a spinal disc (nucleus pulposus) pushes through cracks in the outer ring (annulus fibrosus). That bulging or leakage irritates nearby nerves, causing pain, numbness, or weakness.
What Is a Slipped Disc?
“Slipped disc” is often used interchangeably with “herniated disc.” In strict terms, “slipped” suggests the disc has shifted or bulged—but the result (nerve pressure) is what truly matters. In everyday language, both refer to the same problem: a disc pressing on nerves.
Symptoms Indicating the Need for Surgery
Before we rush to the operating room, certain red flags demand serious attention.
Persistent Pain and Nerve Compression
If pain persists for 6–12 weeks despite rest, physiotherapy or injections, and it interferes with daily life, surgery may become necessary.
Loss of Bladder or Bowel Control
Sudden incontinence or inability to urinate/defecate may signal cauda equina syndrome—an emergency that often mandates prompt surgery.
Progressive Weakness or Numbness
When muscle weakness or numbness steadily increases—especially in legs or arms—it suggests worsening nerve damage. This may push the decision toward surgery.
In short, surgery becomes more likely when your body “reports alarm,” not just mild discomfort.
Diagnostic Approaches
To make the right decision, doctors use a mix of imaging and examinations.
Imaging Techniques: MRI and CT Scans
MRIs are the gold standard. They show disc structure, nerve compression, and the degree of damage. CT scans or CT myelograms help those who can’t do an MRI.
Clinical Evaluation and Neurological Tests
A physician tests reflexes, muscle strength, sensations, and special manoeuvres (e.g. straight leg raise). Sometimes, nerve conduction studies (EMG) add detail. These help confirm how badly nerves are involved.
Treatment Options Before Considering Surgery
Most slipped or herniated discs improve without surgery. In fact, 90% of cases don’t need immediate operative intervention. Let’s first see the non-surgical tools often deployed.
Physical Therapy and Rehabilitation
Stretching, core-strengthening, posture training, and guided exercises help relieve pressure, improve stability, and reduce symptoms over weeks.
Medications and Pain Management
NSAIDs, analgesics, muscle relaxants, and neuropathic pain agents may be prescribed. These ease inflammation and nerve pain while healing occurs.
Epidural Steroid Injections
Targeted injections of corticosteroids near the nerve root reduce swelling and pain. This can “buy time” for healing.
If these fail to yield relief or neurological symptoms worsen, then we begin serious conversations about surgical options.
Surgical Interventions
When non-surgical routes aren’t enough, a surgeon may propose one or more of the following:
Microdiscectomy
The most common herniated disc surgery is for the lumbar (lower back). A small portion of the disc pressing on the nerve is removed via a tiny incision. Benefits: shorter recovery and good success rates.
Spinal Fusion
Used when vertebral instability is present. Two or more vertebrae are fused to eliminate motion at that unstable segment.
Artificial Disc Replacement
Also known as disc replacement surgery. Rather than fusing vertebrae, the damaged disc is replaced with an artificial one. This maintains mobility. Used more often in cervical disc herniation cases.
Minimally Invasive Spine Surgery
These include endoscopic approaches, tubular retractors, and techniques like the TESSYS method (endoscopic disc removal) to reduce soft-tissue damage.
Combined Approaches
Sometimes a surgeon may decompress (remove disc material) + fuse, depending on the degree of damage.
Risks and Benefits of Surgical Treatment
Surgery is not without risk. But with an experienced spine fixation surgeon in Kolkata, the balance often favours benefit—if done for the right reasons.
| Aspect | Benefits | Risks / Downsides |
| Relief of nerve compression | Quicker pain relief, nerve function recovery | Infection, bleeding, anaesthetic risks |
| Faster return to activity | Patients often resume life faster than prolonged conservative treatment | Scar tissue formation |
| Improved strength/function | May reverse weakness or numbness | Possible failure to relieve symptoms |
| Long-term stability | Fusion or disc replacement may reduce recurrence | Adjacent segment degeneration |
Complications are rare but real: nerve injury, cerebrospinal fluid leaks, implant failure, persistent pain, and new disc herniations. Still, in many hands, back pain surgery options achieve excellent outcomes—especially when patients are selected wisely.
Final Thoughts: Making an Informed Decision
Deciding whether surgery is “the only solution” is rarely black-and-white. In many cases, non-surgical paths work well. In others—with worsening neurological signs or persistent pain—surgical paths like lumbar discectomy, cervical disc herniation surgery, or disc replacement surgery may be essential.
Here is a quick decision checklist:
- Try non-surgical methods for at least 6–12 weeks (physical therapy, injections).
- Monitor for red flag symptoms (bowel/bladder changes, worsening weakness).
- If function, quality of life, or nerve health is declining, consult a surgeon.
- Choose someone with advanced experience—someone known as a spine fixation surgeon in Kolkata, for example, who can offer minimally invasive techniques.
Talk with a specialist about your unique situation. Seek second opinions. A careful, patient-centred approach often leads to the best long-term result.
People Also Ask
Can a slipped disc heal by itself?
Yes. Many slipped/herniated discs improve over weeks to months due to natural resorption and reduced inflammation. Conservative treatments often suffice.
How long should you try non-surgical treatment before surgery?
Usually, 6 to 12 weeks of physical therapy, medications, or injections are recommended before evaluating surgical options.
What is the success rate of herniated disc surgery?
Success (relief of symptoms, return to function) is often high, with many patients reporting significant improvement. Some studies show no long-term difference between surgery and conservative treatment, but surgery gives faster relief.
Is minimally invasive spine surgery better than traditional surgery?
It often causes less soft-tissue damage, less pain, and quicker recovery. But the best option depends on patient anatomy, surgeon skill, and severity of the condition.
Can a herniated disc cause permanent damage?
If nerve compression is severe and prolonged, it can lead to lasting weakness or sensory loss. That’s why early evaluation is important.